Lessons from a Pandemic: 1. Digital collaboration and preparedness
[London, 30 April 2020]
The tragic global outbreak of covid-19 has already taught us many severe lessons in pandemic preparedness and response. Rapid innovation and product TTM, distributed collaboration, infection modelling, additive manufacturing of Personal Protective Equipment (PPE), AI-powered vaccine and anti-viral drug development and clinical trials, sharing of real-time research data, scenario modelling and contact tracing. All of these elements, and many more, harness the power and the universal ubiquity of digital. Digital technology is thus at the heart of our fight against the virus.
I hope that, post pandemic, the lessons learnt from this pandemic will persist and a global, shared architecture of advanced digital competencies is permanently established to support more effective collaboration, innovation and a quicker response to better defeat future pandemics, biothreats and other worldwide catastrophes.
In the first article of this series, I discuss how digital technology is powering a positive step-change in global medical collaboration, and the need for our industry and society to establish an effective rapid response capability in time for future pandemics and biothreats.
Ground-up mobilisation, or ‘don’t wait for the politicians!’
SARS-CoV-2, the microscopic virus that causes covid-19, was first reported in Wuhan, a major travel hub in China, in December 2019. It parasitically invades the respiratory tract and already (at the time of writing this article) has resulted in over 230,000 deaths worldwide, with over 26,000 in the UK alone. Borders do not impede its relentless spread and there is yet no proven treatment or vaccine. The WHO officially declared the novel coronavirus a pandemic on 11 March 2020.
Perhaps the most telling revelation of this pandemic is not how quickly covid-19 has spread, China’s sadly predictable duplicity, or most governments’ slow initial reaction, but the lack of any preparedness blueprint and any meaningful global response coordination from the White House. Previous presidents facing epidemiological threats would quickly collar other world leaders to agree a joint, coherent international response. Barack Obama did this during the H1N1 (2009) and Ebola (2014) outbreaks. I do not wish to be political, but Donald Trump’s actions and messages to-date signal an abdication of US leadership in our global fight against the current pandemic.
To be fair to the White House, the WHO has itself failed to add much value or provide clear global coordination. The EU has also proved to be largely incompetent and impotent at this time of crisis. This is acutely illuminating in this year of Brexit. The EU in fact, acting under China’s diplomatic pressure led by Zhang Ming, China’s envoy to the EU, had been wickedly complicit in delaying and redacting its own report into China’s coronavirus disinformation campaign in fear of damaging trade relations. An analyst who contributed to the report, Monika Richter, was quoted in The Times this week, as saying “self-censoring to appease the Chinese Communist Party… will set a terrible precedent and encourage similar coercion in the future”.
As a natural libertarian, I am not unhappy with this catastrophic failure of top down governance and a lack of preparedness by those who are supposed to protect us, even as scientists have for years warned us that a global pandemic was likely. I hope that voters will systematically deal with this in due course through democratic processes. In the meantime, many actors in today’s fight against covid-19, such as scientists, NGOs, healthcare providers and manufacturers, have quickly learnt from this pandemic that they should not wait for government or EU directives. Many private and public entities have self-mobilised, and are pragmatically organising and collaborating across disciplines and borders, whether it is to locally produce PPE kit or repurpose production lines and distribution channels for urgently required medical equipment.
Such mass-scale self-organisation and collaboration would not be possible without the universal brokerage of digital technology and high-speed internet. Most actors currently default to teleworking, using reliable videoconferencing and collaboration tools such as Skype, Zoom, Webex, Microsoft Teams or Slack. Documents and other artefacts are produced efficiently and collaboratively across the globe. Research and statistical data is shared in real time. The outcome has been a much more efficient use of time and resources, a reduction of time-wasting commuting and its environmental impact, and faster decision making (virtual meetings can be organised much faster than physical ones). I sincerely hope that while some regular face-to-face contact may arguably be important for team social cohesion, this new digital workplace ‘normal’ will persist as the default into the future.
Rapid self-organisation and investment
Industry and academia have impressively risen to the challenge, especially here in Britain and the US. New research and innovation, with clear impact pathways, have been fast-tracked to deliver a significant contribution to the understanding and management of the pandemic. This includes rapidly founding multi-disciplinary and collaborative innovation alliances, and the massive upscaling of distributed production of ventilators, PPE, testing kits, antibody therapies and trial vaccines. While some still criticise the UK government’s initially hesitant response, extensive government funding has now been made available for the necessary digital enablers.
Nothing like this has ever been done before. Strategic, multi-$m collaborations typically take years to negotiate, not least because in normal times, intellectual property (IP) rights, licenses and commercial interests need first to be secured by the different parties. Regulatory approval is also typically a laborious and extended process. But these are not normal times. The FDA has already issued emergency approvals for dozens of covid-19 applications and trials. Covid-19 has catalysed the emergence of new models in global cooperation, regulations and investment.
One example is Bill & Melinda Gates Foundation a month ago launching its covid-19 Therapeutic Accelerator, led by the Foundation’s CEO, Mark Suzman and backed by Wellcome and Mastercard. The Accelerator has already secured funding of $125 million to screen a vast number of existing drugs and compounds, which had not been licensed for public use, to test whether they could work on covid-19, and eventually on other diseases.
The Accelerator work, led by the Rega Institute in Belgium, will review some 14,000 compounds sourced from several research and proprietary libraries of pharmaceutical companies, including Merck, Novartis and Pfizer, for efficacy against coronavirus. We thus potentially already could have an effective drug against covid-19. If taken forward post-pandemic, such a digitally-enabled collaboration model is likely to support research on broad-spectrum anti-coronavirus drugs and other panvirals. Libraries of unused drugs, or drugs and vaccines with parallel applications, could be shared and quickly researched with AI-powered analytical tools to identify candidates against new pathogens.
Mark Suzman admits that the current willingness to share proprietary compounds to this degree is “unprecedented”. New, open alliances are springing up like mushrooms after autumn rain. Existing ones are fast refocusing their resources on covid-19. Many are already engaged in salvaging and reformulating encouraging drugs to tackle influenza, coronaviruses, flaviviruses and alphaviruses, such as the federally funded Antiviral Drug Discovery and Development Center (AD3C), initially set up in 2014. The excellently named JEDI (Joint European Disruptive Initiative), funded by AXA Research Fund and Merck, is developing an open source library. On 1 May, it is launching the Billion Molecules against Covid19 Grand Challenge, which aims to screen billions of molecules with blocking interactions relevant to SARS-CoV-2, and rapidly develop treatments.
To illustrate that we could be quite close to an effective therapeutic, Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), has just announced that Gilead Sciences found positive results from early clinical trials of its antiviral remdesivir. Preliminary results demonstrate that patients given the drug exhibited a 31% faster recovery time from covid-19. This result needs to be taken with some initial caution; a separate, peer-reviewed study published in the Lancet, did not find any positive effect of the drug. Other antivirals, such as APN01 in China and Brilacidin from Innovation Pharmaceuticals, are also being tested.
Digitally enabled research
The rapid analysis of compounds, and indeed most biotechnology research, would not be possible without complex digital solutions. Recent advances in digital biosensors and computational approaches have introduced new monitoring and microscopy techniques. Digital holography has emerged as a powerful alternative to conventional bright-field microscopy. Virus, vaccine and antibody drug research, such as dielectric spectroscopy, and production processes, are underpinned by digital biosensors and complex analytical and modelling software. Biochemistry, molecular biology, medical science and research have all been revolutionised by digital.
The rapidly growing interdisciplinary field of bioinformatics develops complex, convergent approaches and tools to screen and analyse huge and complex sets of biological data. It powers today’s drug and vaccine research. Bioinformatics is critically dependent on the power of digital, and the active collaboration between microbiologists, IT experts, data scientists and mathematicians. Translation research in life sciences, that is applying existing knowledge to new areas, usually demands processing huge volumes of candidate data. Without powerful computers, smart software and mathematical modelling, analysing multiple protein sequences or screening millions of samples manually would simply be impossible.
To fast-track human trials, real-time monitoring and analysis needs to rapidly demonstrate the ongoing efficacy and safety profile of the vaccine or drug. In 2018, the European Centre for Disease Prevention and Control (ECDC) published technical guidance on ‘Designing and implementing an immunisation information system’ (IIS), covering the design and application of vaccines. Without a standardised, real-time, shared digital IIS platform, which supports rapid risk assessment and decision making, including prioritising interventions, any quick rollout of mass immunisation would be unfeasible and unsafe.
In the spirit of this new, open collaboration, I hope that such best-of-class systems, collaboration platforms and other digital enablers should be freely shared in the future, in the open source tradition and in the same way that proprietary compounds are currently being shared. This would equip every contributor with the best tools to help us collectively defeat covid-19 and future pandemics.
New paradigms in vaccinology
With some 80 vaccines already in train for human testing, new paradigms in vaccinology are emerging. Conventional vaccines teach the immune system to recognise pathogens, usually by introducing an inert or debilitated form of the virus. But there are new approaches to immunisation rapidly being trialled. For example, mRNA vaccines employ genetic code to instruct cells how to mount an immune response. They are a promising emerging alternative to conventional vaccines, because of their high potency, capacity for rapid development and potential for fast, low-cost manufacture and safe administration.
This is an exciting and fast developing area. For example, favipiravir already targets a protein universal to RNA viruses, such as Ebola and Lassa fever. Similarly, cidofovir, a nucleotide analog, has proven efficacious against DNA viruses such as herpes, polyoma, adeno and pox viruses. Several incumbents and start-ups are exploring the promise of mRNA vaccines, which target the messenger RNA to elicit an immune response. The great advantage of mRNA approach is that adapting the vaccine for specific coronavirus variations is rapid. Moderna, a 2010 start-up, has just created mRNA-1273, a candidate covid-19 vaccine, in merely six weeks.
Scientists have also long identified mRNA vaccines as potential immunisations against cancer, but until covid-19 appeared, there wasn’t much investment available into this technology, and how such vaccines could be produced on a massive scale at an affordable price. A tenacious industry rumour suggests that big pharmaceutical companies in US may have been actively suppressing some mRNA research since they have a significant conflict of interest. Why develop compounds that immunise against cancer, when there are huge profits to be made instead from chemotherapy and immune drugs for cancer treatment? Now under renewed scrutiny, hopefully big pharma will prove this rumour wrong and proceed at pace with research and significant investment into mRNA and other emerging technologies, beyond the immediate treatment of covid-19.
Reverse vaccinology, antigen discovery derived from a pathogen’s genome, is another example of an evolving vaccinology approach, critically dependent on the use of bioinformatics, cloud supercomputing and digital collaboration around the world between scientists, to sequence the DNA of the pathogen and identify possible antigens through mass screening.
Prior to the current pandemic, the WHO had already identified eleven diseases as pandemic risks due to their infectivity and lack of treatments. The WHO and other leading actors, such as the Gates Foundation, have typically focused on research against known and present pathogens and outbreaks. This is a reactive paradigm. Traditionally, there has been little focus and funding on preparedness against a future, as yet unidentified pathogen, i.e. a pre-emptive paradigm.
There are some exceptions, most notably the Coalition for Epidemic Preparedness Innovations (CEPI), a public–private partnership founded in 2017 in the shadow of the earlier Ebola outbreak. With international funding commitments exceeding $650 million, CEPI’s initial focus was on three of the priority diseases on the WHO list; Lassa fever, Nipah and MERS. But it is now pivoting also to research new generations of vaccines against hypothetical pandemics and bioterrorism.
CEPI is coordinating the development of vaccines and aims to produce hundreds of millions of doses available within 12-18 months. It is already working on a fair, needs-based, global allocation system. CEPI’s anti-covid-19 programme is likely to cost some $3 billion. The Therapeutics Accelerator’s programme prioritises the distribution of treatments particularly to emerging economies, deemed most at risk from the pandemic. To produce 100 million doses by the end of 2020, it will need funding of $2.25 billion. Wellcome estimates that at least $8 billion of new funding will be needed for the global response to covid-19 to develop and make treatments universally available.
But to put this breathtakingly substantial investment into perspective, reliable sources quoted in Bloomberg.com estimate the likely cost to the global economy of covid-19 as between $2 trillion and over $4 trillion in lost output, depending on the length of its containment period.
The unknown unknowns
Many prominent scientists have long predicted a global pandemic caused by viral spillover from wild animals to humans. One, Dennis Carroll, set up a research programme under the Obama administration named PREDICT to identify significant zoonoses through biological analysis and predictive modelling. When the USAID founding for this dried up, he went on to create the Global Virome Project (GVP), a collaborative scientific project to discover and prevent yet unknown, future zoonotic viral threats.
In a 2018 paper in Science, Dennis and his team sagely warned us that “outbreaks of novel and deadly viruses highlight global vulnerability to emerging diseases, with many having massive health and economic impacts. Our adaptive toolkit—based largely on vaccines and therapeutics—is often ineffective because countermeasure development can be outpaced by the speed of novel viral emergence and spread”. In the last few weeks, he has gallantly resisted saying, “I told you so!”.
The GVP research highlights that there is likely to be up to 827,000 viruses with the potential to infect people. While most are likely to be benign, many thousands of these could be potentially deadly pathogens, some of which could additionally spread rapidly through human-to-human transmission. Many lethal virus families have already been identified, such as several highly virulent, haemorrhagic fever causing pathogens. Just one of these, Marburg, whose outbreak in Germany and Serbia was thankfully contained, proved to have a fatality ratio of up to nearly 90%.
This challenge is fuelling a welcome refocus of researchers and investment, catalysed by the covid-19 pandemic, from funding profit-conscious responses to specific pathogens such as MERS or SARS-1, to broad-spectrum, panviral drugs and vaccines, in readiness for future pandemics. Effective management of virus genome sequencing work globally requires a digitally enabled collaboration platform and long-term international investment, on the scale probably similar to the Human Genome Project, which had funding from multiple sources and was performed across some twenty universities and research centres in the US, UK, Japan, France, Germany and China.
Many scientists have been warning us of global threats likely to occur in our lifetimes. The response structures emerging from covid-19 should persist and regularly rehearse future pandemics and responses, simulating outbreaks and bioterrorism attacks. Digital technology allows complex scenario and risk modelling, and supports response evaluation and planning.
One of the key takeaways from the covid-19 pandemic, is how badly prepared our governments and societies were for this. We regularly perform drills, so that we know how to safely evacuate buildings in the event of fire. Governments regularly invest $-billions in conventional wargaming and cyber security/warfare. There simply has never been a similar scale of investment on rehearsing and preparing a coherent, rapid response to a sudden pandemic or other biothreats.
Let’s draw lessons from Japan’s tsunami preparedness. Its Meteorological Agency (JMA) employs a dense network of sensors and an information system that gives nationwide tsunami warnings within three minutes. Community level Disaster Preparedness offices continuously educate the population through community awareness and outreach programmes, and response drills. When required, they coordinate evacuations. Given the scale of human and economic destruction that covid-19 has inflicted upon us, surely we need to develop a similar, science-based and socially accepted rapid response capability, and repair or even replace the broken organisations that have so catastrophically failed to protect us, such as the WHO and several structures within the EU.
In summary
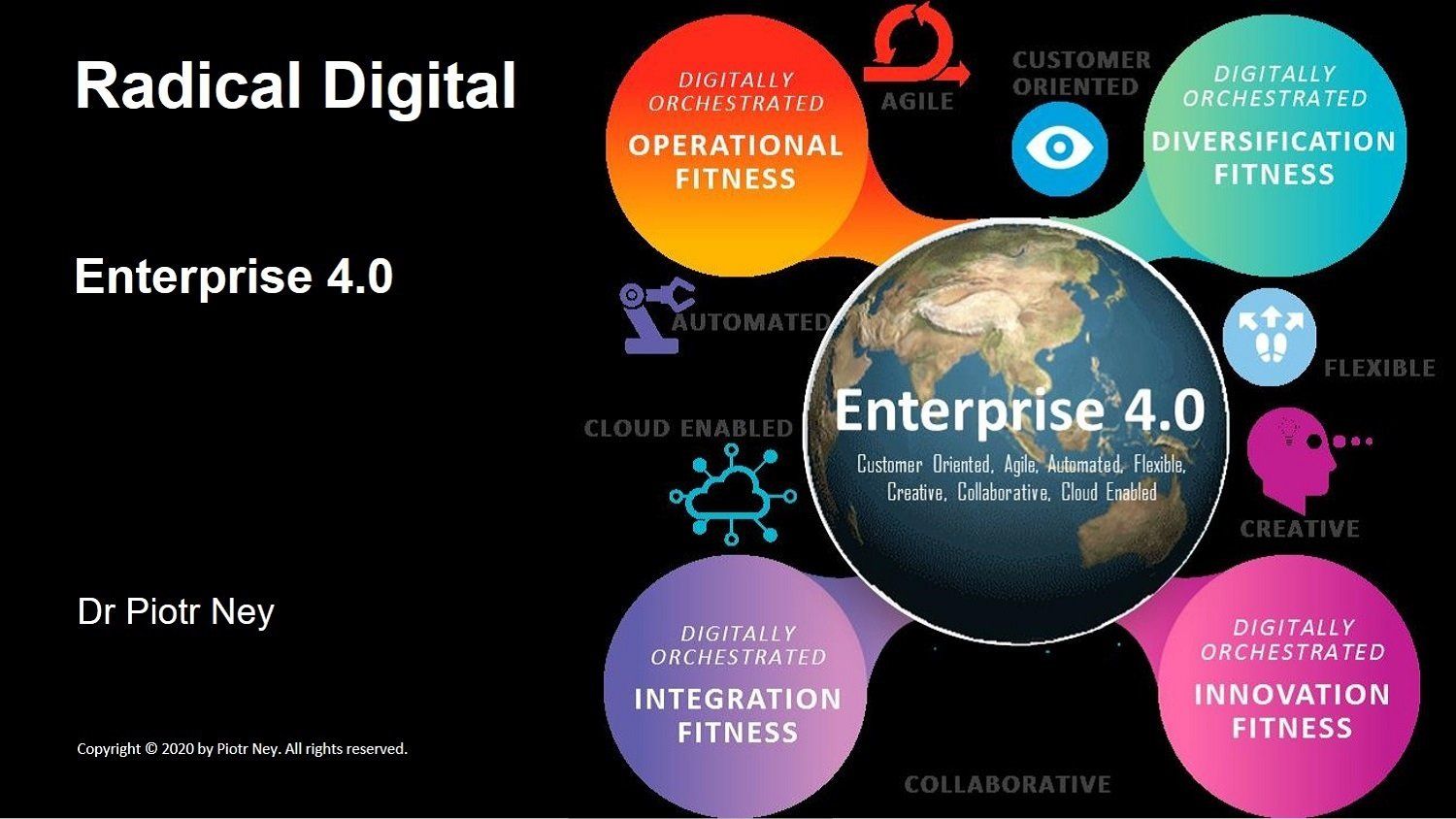
Digital technology allows us to rapidly and dynamically reconfigure our global capabilities and resources, as well as engage new paradigms, to tackle sudden discontinuities, such as an unforeseen pandemic. Digitalisation, automation and rapidly evolving information technologies have enabled new, cloud-based collaboration models to tackle such threats with agility. Our digital economy is definitely more resilient and better positioned today to fight a novel global threat, than the hard-coded, physically-oriented and rigid archetypes of previous industrial cycles.
Digital supports scientific research and drug development. It catalyses the seamless, 24/7 global collaboration of multiple, cross-disciplinary actors to fast-track outcomes, through co-creation, productivity and workflow tools. AI and robotics automate and greatly speed up routine tasks and processes. Open data sources, distributed ledger technology (blockchain) and advanced data mining techniques, allow us effectively and safely to share previously inconceivable volumes of clinical evidence and other information. And increasingly, such mass collaboration and data sharing are performed in the cloud, enabling actors who have limited up-front capital budgets or access to advanced computational capacity to readily join in.
Digital biosensors, whether in the lab, clinical trials or symptom tracking in the community, continually report in real-time what is happening. Advanced AI-enabled diagnostics give early warnings of complications. Complex digital modelling tools combine sensor data with numerous other sources to give us insight into emerging developments and help us prioritise interventions. Digital algorithms help us predict outcomes and optimise processes, such as the global distribution of equipment and eventual drugs and vaccines.
Social media, when harnessed positively, is also an all-powerful tool to share accurate information and guidance, dispel misinformation, impart health advice and nudge people towards desired behaviours. Its role needs to be designed into any future rapid response blueprint.
While digital is no doubt the critical backbone to our response to the pandemic, ultimately it is only a technology, a tool in our hands. For it to truly prove its potential and to serve us better in the post-pandemic future, several significant structural and societal hurdles need to be overcome. For this, we need to develop a persistent political will and a new, digital-empathetic social contract, not least in the areas of personal privacy and social media accountability.
I am encouraged by how effectively individuals and enterprises, private and public, have mobilised and established collaborations and networks as a response to covid-19. Rapid government funding, not least here in the UK, and a widespread relaxation of the usual protocols, investment appraisals, legal, regulatory and compliance hurdles, have all greatly supported this.
This new paradigm is unlikely to survive fully beyond this pandemic. People and organisations often have frustratingly short memories. Once the adrenaline rush is over, some funders are likely to dust off their former investment appraisal mechanisms. Regulators are likely to retighten their scrutiny. Politicians will refocus on other priorities, not least the massively damaged economy and rising unemployment, and the next election cycle. We will return to our factories, offices and schools.
Yet covid-19, even in these early weeks, has already taught us some invaluable lessons in what we can jointly achieve leveraging the disruptive power of digital. It has shown us what the new ‘normal’ could look like, and what is possible when we cooperate liberally and effectively on a global scale to tackle common threats, in a smart, distributed, people-centric and environmentally positive way. It has also demonstrated that we need to invest in regularly rehearsing our response to any future pandemics, and as yet undiscovered pathogens.
I optimistically believe that some of this new global paradigm and awareness will persist, and the covid-19 pandemic will help guide us a little way towards a new, better ‘normal’, our digitally-enriched and safer future.
Dr Piotr Ney is an energetic promoter of innovation, digital transformation, customer and operational excellence, and sustainability, with some thirty five years of change leadership, consultancy and senior executive experience. He has an MBA in International Business and a PhD in Economics and Management, lectures part-time in Innovation Management and Disruptive Strategy and is a popular speaker at global business events. Piotr works in London and internationally as an independent consultant and educator.
Copyright © 2020 by Piotr Ney. All rights reserved. No part of this work may be published, reproduced or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission of the author.